Understanding the Basics: What Is a Euploid Embryo?
The Definition of a Euploid Embryo
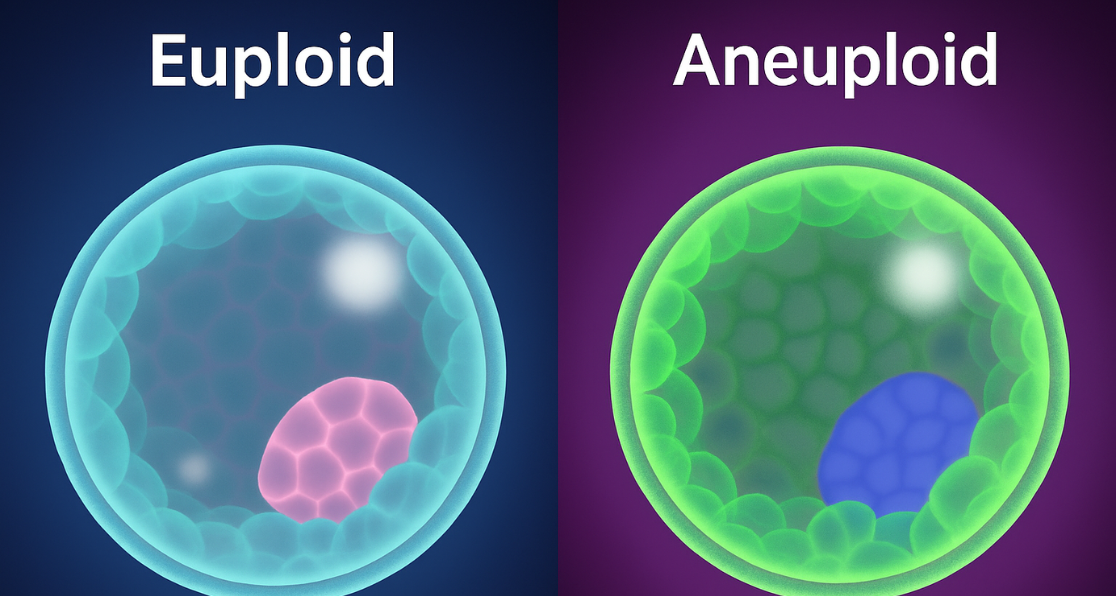
A euploid embryo represents the gold standard in assisted reproduction—it contains the correct number of chromosomes necessary for healthy development. Specifically, a euploid embryo possesses 46 chromosomes arranged in 23 pairs, with one chromosome from each biological parent contributing to each pair. This complete chromosomal complement is essential for normal embryonic development and significantly increases the likelihood of a successful pregnancy. When comparing euploid vs aneuploid embryos, the genetic integrity of the former makes all the difference in IVF success.
Chromosomal Structure in Euploid Embryos
Human cells contain 22 pairs of autosomal chromosomes (numbered 1 through 22) and one pair of sex chromosomes that determine biological gender. In euploid individuals, the chromosome formula is 46, XX for females and 46, XY for males. When embryologists identify a euploid embryo through genetic testing, they’re confirming that this embryo has the optimal genetic foundation for developing into a healthy baby.
Success Rates with Euploid Embryo Transfer
The importance of transferring a euploid embryo cannot be overstated. Research demonstrates that euploid embryos achieve implantation rates ranging from 60% to 80%, compared to 50% to 65% for untested embryos. Furthermore, live birth rates for euploid embryo transfers can reach up to 70%, with some studies reporting that individuals with three chromosomally normal embryos have a remarkable 94.9% chance of achieving pregnancy.
Aneuploidy vs Euploidy: The Critical Distinction
Defining the Key Differences
Understanding aneuploidy vs euploidy is fundamental to grasping why some IVF cycles succeed while others fail. While euploidy represents chromosomal normalcy, aneuploidy refers to an abnormal number of chromosomes—either too many (trisomy) or too few (monosomy). This distinction between aneuploidy vs euploidy directly impacts embryo viability and pregnancy outcomes. Comprehensive knowledge of euploid vs aneuploid embryos helps parents make informed decisions about genetic testing.
Comparing Pregnancy Outcomes
When comparing aneuploidy vs euploidy, the differences are stark. Aneuploid embryos are significantly more likely to result in implantation failure, with studies showing they account for 40% to 75% of pregnancy losses. In contrast, euploid embryos demonstrate superior reproductive potential across all metrics, including higher implantation rates, reduced miscarriage rates, and a greater likelihood of healthy live births.
Age-Related Aneuploidy Patterns
The prevalence of aneuploidy varies considerably with maternal age. In women under 35, approximately 59% to 73% of embryos test as euploid. However, this percentage drops dramatically as women age—falling to 50-56% for women aged 35-37, 37-46% for ages 38-40, and below 30% for women over 41. This age-related increase in aneuploidy rates underscores the importance of understanding aneuploidy vs euploidy when planning fertility treatment.
What Causes Aneuploid Embryos?
Errors During Cell Division
The formation of aneuploid embryos primarily results from errors during cell division, particularly during meiosis—the process by which egg and sperm cells develop. These chromosomal abnormalities can originate from either maternal or paternal sources, though maternal age represents the most significant risk factor.
The Impact of Maternal Age
As women age, their eggs age alongside them. A 35-year-old woman’s eggs have also existed for 35 years, making them increasingly susceptible to chromosomal segregation errors. This age-related decline in egg quality explains why aneuploidy rates increase exponentially after age 35, with women over 40 experiencing aneuploidy rates exceeding 50%. Understanding the distinction between euploid vs aneuploid embryos becomes increasingly critical for women over 35.
Additional Contributing Factors
Beyond maternal age, several additional factors contribute to aneuploidy. These include errors during sperm formation, though paternal age shows less correlation with aneuploidy than maternal age. Mitotic errors after fertilization can also create aneuploid cells in developing embryos, leading to a condition called mosaicism, where both normal and abnormal cells coexist.
Environmental and Lifestyle Influences
Environmental and lifestyle factors may also play a role. Research suggests that smoking, excessive alcohol consumption, obesity, and certain dietary factors can increase the risk of chromosomal abnormalities in both eggs and sperm. While these lifestyle factors represent modifiable risk factors, the predominant cause of aneuploidy remains the natural aging process of oocytes.
Common Types of Aneuploid Conditions
Autosomal Trisomies
Understanding specific aneuploid conditions helps illustrate the real-world implications of aneuploidy vs euploidy. The most recognizable aneuploid condition is Down syndrome, or trisomy 21, where individuals possess three copies of chromosome 21 instead of the normal two. Approximately 1 in 700 live births results in Down syndrome, with risk increasing dramatically with maternal age—from 1 in 2,500 for mothers under 20 to 1 in 25 for mothers over 40.
Other trisomy conditions include Edwards syndrome (trisomy 18) and Patau syndrome (trisomy 13), both of which typically result in severe developmental abnormalities and shortened life spans. Most trisomies, however, result in early pregnancy loss, with studies estimating that trisomies cause approximately 35% of all miscarriages.
Sex Chromosome Aneuploidies
Sex chromosome aneuploidies present different outcomes. Turner syndrome (monosomy X, or 45, X) occurs when a female has only one X chromosome. This condition, while compatible with life, causes various developmental challenges, including short stature and infertility. Klinefelter syndrome (47, XXY) affects males who have an extra X chromosome, potentially causing developmental and fertility issues.
The Role of PGT-A in Identifying Euploid Embryos
What Is PGT-A Testing?
Preimplantation Genetic Testing for Aneuploidy (PGT-A) represents the most advanced method for distinguishing euploid from aneuploid embryos before transfer. This sophisticated genetic screening occurs during IVF treatment, allowing fertility specialists to select euploid embryo candidates with the highest potential for successful implantation and healthy development. PGT-A is essential for identifying euploid vs aneuploid embryos with precision.
The PGT-A Process Step-by-Step
The PGT-A process involves several carefully orchestrated steps. After egg retrieval and fertilization, embryos develop in the laboratory until day 5 or 6, when they reach the blastocyst stage. At this point, embryologists perform a trophectoderm biopsy, removing a small sample of cells from the outer layer of the embryo that will eventually become the placenta. Crucially, this biopsy does not affect the inner cell mass that develops into the baby.
Analyzing and Interpreting Results
The biopsied cells undergo comprehensive chromosomal analysis using next-generation sequencing (NGS) technology, which can detect numerical abnormalities across all 24 chromosome types. Results typically return within 7-10 days, classifying each embryo as euploid (chromosomally normal), aneuploid (chromosomally abnormal), or mosaic (containing both normal and abnormal cells).
PGT-A Accuracy and Limitations
Understanding Test Accuracy
While PGT-A represents a powerful tool for embryo selection, understanding its accuracy helps set realistic expectations. Most sources report PGT-A accuracy exceeding 97%, though some studies suggest the test correctly identifies chromosomal abnormalities approximately 84% of the time. This variance reflects the complexity of interpreting genetic data and the biological reality of embryonic mosaicism.
The False Positive Problem
False positive results—where viable euploid embryos are incorrectly classified as aneuploid—present one of PGT-A’s most significant limitations. Studies suggest that 40% of embryos flagged as abnormal may actually be viable, potentially resulting in the unnecessary discarding of embryos with developmental potential. This false-positive rate underscores the importance of viewing PGT-A as a screening tool rather than a definitive diagnostic test.
False Negative Considerations
False negatives, where aneuploid embryos are mistakenly identified as euploid, occur less frequently but carry serious implications. Depending on the study, false-negative rates range from 0.1% to 23%, with the overall chance of misdiagnosis per embryo transfer estimated at approximately 0.2%. This means roughly 2 in 1,000 presumed euploid embryos may actually be aneuploid, potentially explaining some pregnancy losses or failed implantations.
Challenges with Mosaic Detection
The accuracy of PGT-A for mosaic embryos remains particularly controversial. These embryos, containing both normal and abnormal cells, present diagnostic challenges because the trophectoderm biopsy may not accurately reflect the chromosomal status of the inner cell mass. Some mosaic embryos can develop into healthy pregnancies, while others may fail to implant or result in miscarriage.
Mosaic Embryos: The Gray Area
What Are Mosaic Embryos?
Mosaic embryos represent a third category beyond aneuploidy vs euploidy, characterized by containing both chromosomally normal and abnormal cells. Modern PGT-A technology can detect mosaicism, typically defined as embryos with 20% to 80% abnormal cells. This intermediate classification creates difficult decisions for IVF patients who may have mosaic embryos as their only option for transfer.
Clinical Outcomes with Mosaic Transfers
Clinical outcomes for mosaic embryo transfers fall between those of euploid and aneuploid embryos. Research indicates that mosaic embryo transfers result in significantly lower clinical pregnancy rates (approximately 40% versus 59% for euploid embryos) and higher miscarriage rates (33% versus 20% for euploid embryos). However, numerous healthy babies have been born from mosaic embryo transfers, with over 100 live births documented showing no abnormal phenotypes.
Factors Affecting Mosaic Embryo Success
The level of mosaicism appears to influence outcomes, with low-level mosaic embryos (containing less than 40-50% abnormal cells) generally performing better than high-level mosaic embryos. Additionally, the type of chromosomal abnormality matters—segmental abnormalities typically have better prognoses than whole-chromosome aneuploidies.
Prenatal Testing After Mosaic Transfer
For patients considering mosaic embryo transfer, comprehensive genetic counseling and prenatal testing become essential. Amniocentesis or chorionic villus sampling during pregnancy can confirm the chromosomal status of the developing fetus, providing reassurance or allowing informed decision-making.
Improving Your Chances: Lifestyle and Treatment Considerations
Lifestyle Modifications for Better Embryo Quality
While chromosomal abnormalities cannot be completely prevented, several strategies may help optimize embryo quality and improve the proportion of euploid embryo production. Maintaining a healthy lifestyle before and during fertility treatment represents the most accessible intervention.
Specific Nutritional and Health Recommendations
Specific recommendations include consuming a well-balanced diet rich in folic acid and B vitamins, maintaining a healthy body weight, engaging in regular moderate physical activity, and avoiding harmful substances, including tobacco, excessive alcohol, and illicit drugs. For men, research suggests that lifestyle factors, including coffee consumption patterns, obesity, and even underwear choices, may influence sperm chromosomal health, though these associations require further validation.
Preconception Health Optimization
Preconception health optimization should ideally begin several months before fertility treatment. Women should ensure adequate intake of prenatal vitamins containing folic acid, vitamin D, and other essential nutrients. Some evidence suggests that antioxidants like CoQ10 may support egg quality, though recent research has questioned the strength of this effect.
Optimizing IVF Protocols
For IVF patients, working closely with experienced fertility specialists to optimize ovarian stimulation protocols can maximize the number of eggs retrieved, thereby increasing the statistical likelihood of obtaining at least one euploid embryo. Research indicates that women aged 35-37 need approximately 5 oocytes, women 38-40 need about 7 oocytes, and women 41-42 require roughly 10 oocytes to have a reasonable chance of obtaining one euploid embryo.
What to Expect During Embryo Transfer
The Transfer Procedure
Whether transferring a euploid embryo identified through PGT-A or an untested embryo, proper preparation for the transfer procedure can optimize outcomes. The transfer process itself is relatively quick and typically painless, similar to a Pap smear.
Preparing Your Uterus for Transfer
Before transfer, patients undergo endometrial preparation using either hormone replacement therapy or natural cycle monitoring to ensure the uterine lining is optimally receptive. For frozen euploid embryo transfers, this preparation creates an artificial implantation window, synchronizing the endometrium with the developmental stage of the thawed embryo.
Medication Management
Medication compliance is crucial during the transfer cycle. Patients receive progesterone supplementation and sometimes additional hormones to support early pregnancy development. Organizing medications in advance and ensuring reliable access to all prescribed treatments helps reduce stress and ensures optimal preparation.
Post-Transfer Care and the Two-Week Wait
Following the transfer, most clinics recommend modified activity for 24-48 hours, though extensive bed rest is no longer considered necessary or beneficial. The “two-week wait” until pregnancy testing begins can be emotionally challenging, but understanding that the euploid embryo’s fate is largely determined by factors beyond your control can help manage anxiety.
Age and Euploid Embryo Transfer Success
Maternal Age Effects Beyond Chromosomes
An important consideration that challenges assumptions about euploid embryo transfers involves the impact of maternal age at the time of transfer. While PGT-A eliminates embryonic chromosomal abnormalities as a variable, research demonstrates that maternal age still influences outcomes even when transferring confirmed euploid embryos.
Age-Specific Success Rates
Studies show that pregnancy rates after euploid embryo transfer decrease with advancing maternal age, from approximately 72% in women under 38 to about 60% in women over 45. Live birth rates follow a similar pattern, declining from approximately 57% in women under 38 to 40% in women over 45. These differences persist despite transferring chromosomally normal embryos, suggesting that the uterine environment and other age-related factors beyond embryo genetics influence IVF success.
Implications for Treatment Planning
This age-related decline in euploid embryo transfer success, though less dramatic than the decline in euploidy rates themselves, has important implications for treatment planning and patient counseling. It demonstrates that while identifying euploid embryos through PGT-A provides significant advantages, it does not eliminate age-related fertility challenges.
The Bottom Line: Making Informed Decisions
The Value of Understanding Genetics
Understanding aneuploidy vs euploidy empowers IVF patients to make informed decisions about genetic testing, embryo selection, and treatment expectations. While the terminology may seem overwhelming initially, grasping these fundamental concepts helps demystify the IVF process and enables more productive conversations with your fertility team.
When PGT-A Testing Makes Sense
For most IVF patients, particularly those with advanced maternal age, recurrent pregnancy loss, or multiple failed transfers, PGT-A testing offers valuable information for optimizing embryo selection and improving success rates. The ability to identify euploid embryo candidates allows for confident single embryo transfer, reducing multiple pregnancy risks while maintaining or even improving pregnancy rates.
Considering the Limitations
However, PGT-A is not appropriate for every patient or situation. The procedure adds cost, requires embryo freezing, and may not benefit younger patients with large numbers of high-quality embryos. Additionally, the false-positive rate means some viable embryos may be unnecessarily excluded from transfer consideration.
Your Path Forward
Ultimately, decisions regarding PGT-A testing and embryo selection should be made in collaboration with your fertility specialist, taking into account your unique medical history, age, embryo availability, and personal preferences. Armed with an understanding of euploid embryo biology and the implications of aneuploidy vs euploidy, you can navigate these complex decisions with confidence, knowing you’re taking evidence-based steps toward achieving your dream of parenthood. The journey through IVF is challenging, but mastering the concepts of euploid vs aneuploid embryos provides the foundation for success.