Introduction
Imagine lying in bed, drifting into the deepest stages of sleep—only to stop breathing, again and again, without a single snore. No rattling airway, no gasping for air—just silence. This chilling pause, invisible but relentless, defines central sleep apnea (CSA), a sleep-related breathing disorder that affects nearly 1% of adults over 40. Unlike its more notorious cousin, obstructive sleep apnea, CSA isn’t caused by a physical blockage. Instead, it’s the brain’s failure to send the “breathe now” signal to your respiratory muscles—an eerie breakdown of your most fundamental life rhythm.
Decoding Central Sleep Apnea
At its core, central sleep apnea is about communication gone awry. Normally, your brainstem monitors blood gas levels and directs your diaphragm and chest muscles to breathe. In CSA, that conversation stalls. Breathing ceases until carbon dioxide rises enough to force the signal back on—an unsettling cycle that can repeat dozens of times per night.
Primary vs. Secondary CSA
- Primary (Idiopathic) CSA
A rare form with no clear cause. The brain’s respiratory control simply misfires. - Secondary CSA
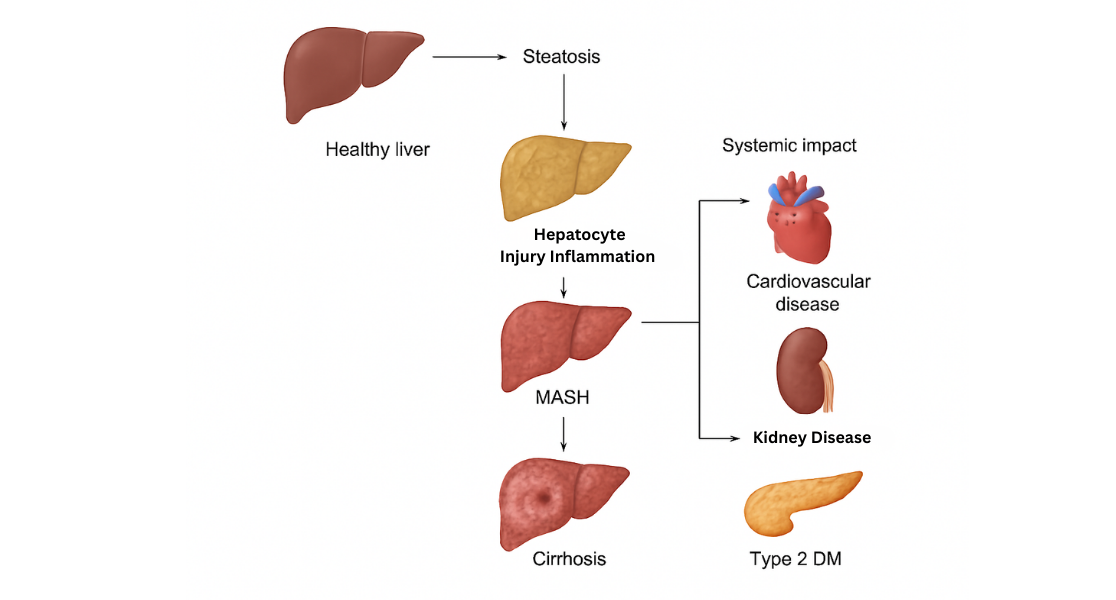
Triggered by another condition—heart failure, stroke, kidney disease, or certain medications such as opioids and benzodiazepines. - Cheyne-Stokes Breathing
A hallmark pattern in many heart-failure patients: crescendo-decrescendo breaths followed by long pauses.
The Silent Alarm: Spotting Symptoms
CSA often hides in plain sight. Many sufferers never wake up gasping—you might not even snore. Instead, look for these subtle clues:
- Excessive Daytime Sleepiness that drags you through morning meetings
- Insomnia and waking repeatedly, despite feeling exhausted
- Morning Headaches signal low overnight oxygen
- Trouble concentrating and mood swings from fragmented rest
- Reported Breathing Pauses by a bed partner, sounding eerily calm rather than obstructed
If you or your loved one notes these signs, it’s time to investigate further.
Diagnosing the Unnoticed: The Sleep Study
To confirm CSA, sleep specialists turn to polysomnography—a comprehensive sleep study performed in a lab. Sensors track:
- Brain waves and sleep stages
- Diaphragm and chest movement (respiratory effort)
- Airflow through the nose and mouth
- Blood oxygen levels and heart rhythm
This overnight investigation reveals how often your breathing stops and whether it’s central in origin or mixed with obstructive events.
Unraveling the Causes: Who’s at Risk?
While anyone can develop CSA, certain factors raise the stakes:
- Age Over 65, when respiratory control can weaken
- Male Sex, possibly due to testosterone’s effect on carbon dioxide sensitivity
- Heart Conditions like congestive heart failure and atrial fibrillation
- Neurological Disorders such as stroke or brainstem injury
- Opioid Use, which depresses the respiratory drive
Identifying underlying causes is essential—treating the root often eases the breathing pauses.
Confronting the Invisible Enemy: Treatment Options
Central sleep apnea demands a tailored approach. If a reversible cause exists—such as a medication side effect or high-altitude exposure—correcting it may restore normal breathing. When pauses persist, these therapies can help:
- Positive Airway Pressure (PAP) Therapy
Adaptive servo-ventilation (ASV) adjusts pressure support breath by breath, keeping your lungs filled and your brain engaged. - Supplemental Oxygen
Boosting nighttime oxygen can stabilize breathing patterns when PAP alone falls short. - Medications
Drugs like acetazolamide stimulate respiratory drive, though side effects require close monitoring. - Phrenic Nerve Stimulation
A surgically implanted device sends gentle pulses to the diaphragm, reigniting each breath from within.
Living Beyond the Pauses
A CSA diagnosis can feel unnerving, but understanding and treatment bring relief. To navigate life with central sleep apnea:
- Educate yourself about your condition and its triggers
- Avoid Sedatives such as alcohol or opioids that worsen breathing control
- Maintain Regular Follow-Ups to adjust therapy, monitor heart health, and optimize sleep quality
With the right support, those silent pauses can transform from a nightly threat into a manageable rhythm—allowing you to reclaim the restorative sleep your body craves.