Understanding Pinguecula: Guide to This Common Eye Condition
Pinguecula is a common, benign eye growth that affects millions of people worldwide, particularly those who spend significant time outdoors. Whether you’ve noticed a yellowish patch in your eye during a routine eye examination or you’re concerned about a small bump on the white part of the eye, understanding this condition is essential for maintaining optimal eye health. This comprehensive guide explores everything you need to know about pinguecula, including its causes, symptoms, diagnosis, and effective management strategies.
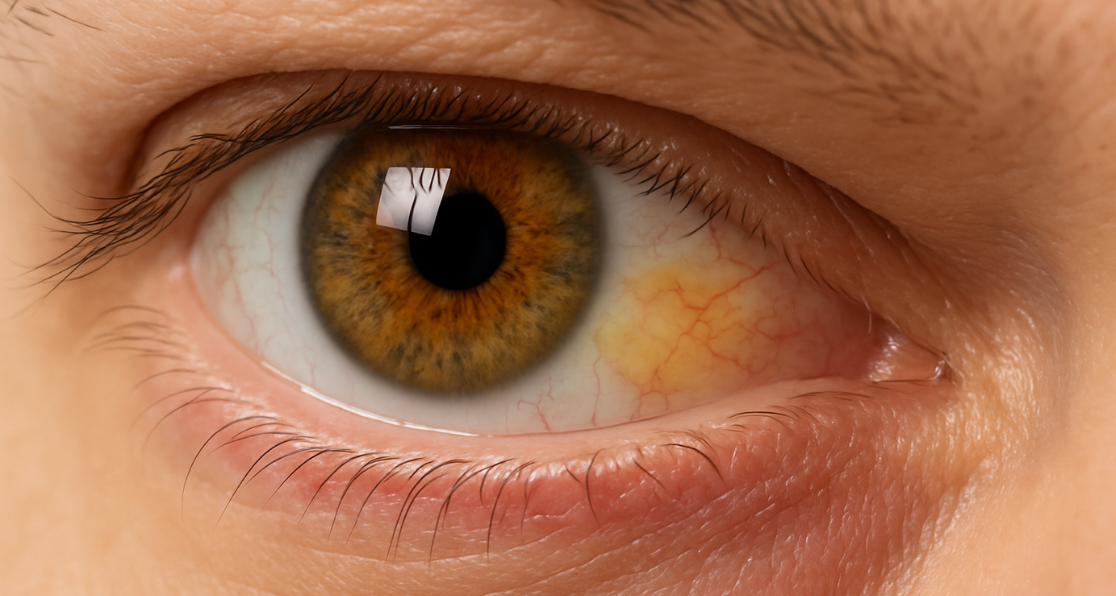
What Is Pinguecula? Defining This Eye Growth
Pinguecula (pronounced pin-GWEK-yoo-lah) is a non-cancerous growth that develops on the conjunctiva—the clear, thin tissue that covers the white part of the eye known as the sclera. This yellowish patch in the eye typically appears as a small, slightly raised bump located on the inner side of the eye, closest to the nose. The growth consists of deposits of protein, fat, and calcium that accumulate in the conjunctival tissue over time. Unlike similar eye conditions, pinguecula remains confined to the conjunctiva and does not grow across the cornea. This characteristic distinguishes it from a related condition called pterygium, which can potentially progress and affect vision. Most individuals with pinguecula experience no vision problems, though the condition requires monitoring to ensure it doesn’t develop complications.
The Three Primary Causes of Pinguecula Development
Understanding what causes pinguecula is crucial for prevention and management. Research has identified several interconnected factors that contribute to the development of this yellowish patch in the eye.
Ultraviolet Radiation Exposure: The Primary Risk Factor
The most significant contributor to pinguecula formation is chronic exposure to ultraviolet (UV) radiation from sunlight. UV rays, particularly UVA and UVB wavelengths, penetrate the eye’s delicate tissues and cause cumulative damage to the conjunctiva. This damage triggers cellular changes that lead to the formation of eye growths on white of the eye. Individuals who work outdoors—including farmers, fishermen, construction workers, and outdoor enthusiasts—face significantly elevated risks. Studies indicate that outdoor occupational activity increases the likelihood of developing pinguecula by more than five times compared to those with minimal sun exposure. Even incidental exposure accumulates over decades, making UV protection essential throughout life, not just during peak summer months.
Environmental Irritants: Dust, Wind, and Dry Climates
Beyond UV radiation, environmental factors play a substantial role in pinguecula development. Chronic exposure to dust, sand, and wind irritates the ocular surface and compromises the natural protective mechanisms of the eye. Individuals living in or frequently visiting dry, arid climates experience higher rates of pinguecula formation due to the combined effects of low humidity, increased particulate matter, and greater UV intensity at higher altitudes. Contact with harsh environmental conditions triggers inflammation and oxidative stress in the conjunctival tissue. This inflammatory response activates cellular processes that contribute to the accumulation of abnormal deposits, gradually transforming the conjunctiva into what we recognize as a bump on the white part of the eye.
Age and Individual Susceptibility Factors
Age represents another critical risk factor for pinguecula development. Research demonstrates that pinguecula prevalence increases substantially with advancing age. While some individuals in their 40s may develop the condition, prevalence becomes significantly higher in those over 50 years old. Studies from various populations show that by the time individuals reach their 80s, most show some evidence of pinguecula.
Gender differences
Also emerge in population studies, with men showing higher prevalence rates—typically 56-70%—compared to women (42-54%). This difference likely reflects occupational exposure patterns and behavioral factors rather than inherent biological susceptibility. Genetic predisposition, smoking history, and individual tear film characteristics also influence who develops this condition.
Recognizing Pinguecula: Symptoms and Visual Signs
One of the most important aspects of managing any eye condition is recognizing early warning signs. Pinguecula symptoms vary considerably among individuals, ranging from completely asymptomatic to moderately bothersome.
Visible Characteristics of Pinguecula
The most obvious sign of pinguecula is the appearance of a small, yellowish or whitish bump on the conjunctiva, typically appearing on the nasal side of the eye (between the cornea and inner corner of the eye). The growth usually measures 2-3 millimeters in diameter, though some cases show larger formations. The bump has a slightly raised, chalky, or fatty appearance and lacks the blood vessels characteristic of pterygium, appearing white or pale yellow rather than pink or red. Images of pinguecula typically show this distinctive yellowish appearance, though the exact coloration varies based on the composition of deposits. Some deposits appear more white than yellow, while others have a more pronounced amber hue. The consistency remains firm, and the surface may occasionally show slight surface irregularities.
Common Symptoms Associated with Pinguecula
- Many individuals with pinguecula experience no symptoms whatsoever, discovering the condition only during routine eye examinations. However, when symptoms do occur, they typically include mild to moderate discomfort rather than severe pain.
- Dry eye sensation ranks among the most frequently reported symptoms. The presence of a pinguecula can disrupt normal tear film distribution across the eye’s surface, leading to areas of dryness and irritation. Some patients describe a foreign body sensation—the persistent feeling that something is in the eye—even though the pinguecula itself doesn’t penetrate the eye surface.
- Mild redness and conjunctival irritation may become apparent, particularly following exposure to environmental irritants, dust, or wind. These symptoms typically worsen during dry weather, in air-conditioned environments, or after prolonged screen time, which reduces blinking and tear production.
When Pinguecula Becomes Inflamed
- In some cases, a pinguecula develops inflammation, a condition called pingueculitis. During inflammatory episodes, the growth becomes more pronounced, redness intensifies, and discomfort increases significantly. Dry eye symptoms often worsen during these flare-ups, and some patients report mild pain or burning sensations.
- Inflammation typically occurs following specific triggers, including prolonged sun exposure, exposure to harsh environmental conditions, contact lens use without proper care, or even minor ocular trauma. Understanding these triggers helps individuals modify their environment and behavior to minimize uncomfortable episodes.
Distinguishing Pinguecula from Pterygium
Given the visual similarities between these two eye conditions, many individuals confuse pinguecula with pterygium. However, important distinctions exist that affect management and long-term outlook.
Key Differences Between These Conditions
While both pinguecula and pterygium develop on the conjunctiva in response to UV exposure and environmental stress, their characteristics differ significantly. Pinguecula appears as a small, yellowish bump that remains localized to the conjunctiva and does not progress toward the cornea. The growth typically stabilizes in size, growing very slowly or not at all over many years. Pterygium, conversely, presents as a fleshy, triangular, pink or red tissue with visible blood vessels that actively grows onto the cornea. This progressive growth can alter the cornea’s shape, induce astigmatism, and potentially impair vision.
The presence or absence of visible blood vessels
Provides an important diagnostic clue. Pinguecula lacks prominent blood vessels on its surface, appearing pale and avascular. Pterygium typically displays numerous dilated blood vessels, giving it a distinctive vascular appearance. Additionally, pterygium often causes more pronounced redness, foreign body sensation, and progressive visual symptoms compared to the generally asymptomatic or mildly symptomatic nature of pinguecula.
Understanding Progression and Vision Impact
Perhaps the most clinically significant difference involves potential vision impact. Pinguecula rarely affects vision because it doesn’t grow across the cornea, which is essential for clear sight. Many individuals live their entire lives with an undiagnosed pinguecula because the condition never causes noticeable visual problems. Pterygium, by contrast, can potentially affect vision if it grows sufficiently to cover the visual axis or alter corneal shape. This distinction makes accurate diagnosis important, particularly when symptoms are present, as management strategies differ considerably between these conditions.
Diagnosis of Pinguecula: What to Expect
Proper diagnosis ensures appropriate management and helps rule out more serious ocular conditions that might require intervention.
The Diagnostic Process
- Eye care professionals typically diagnose pinguecula through a comprehensive clinical examination. During a routine eye exam, your ophthalmologist or optometrist will examine the eye using a slit lamp—a specialized microscope that provides magnified views of ocular structures. The distinctive appearance of a pinguecula under slit lamp examination usually allows immediate identification without requiring additional testing.
- The examination typically includes assessment of the growth’s size, location, and any associated inflammation. Your eye care provider will also evaluate tear film quality and check for dry eye syndrome, which frequently accompanies pinguecula. When necessary, sophisticated imaging techniques, including anterior segment optical coherence tomography (OCT), may document the precise dimensions and depth of the growth, particularly if surgical removal is being considered.
- Your eye care professional will inquire about symptoms, occupational history, sun exposure patterns, and any family history of eye conditions. This information helps confirm the diagnosis and allows for the development of an appropriate management strategy tailored to your specific situation.
Comprehensive Management Strategies for Pinguecula
The good news is that pinguecula responds well to various management approaches, with treatment options ranging from simple at-home care to surgical intervention in rare cases.
Conservative Management and Symptom Relief
Most individuals with pinguecula require no treatment beyond monitoring and symptom management. For those experiencing mild symptoms, several effective strategies provide relief.
- Artificial tears and lubricating eye drops form the foundation of conservative management. Preservative-free formulations work best, as they can be used frequently without irritating the eye. Regular application of artificial tears maintains ocular surface moisture, reduces inflammation, and alleviates associated dry eye symptoms. Many patients find that using lubricating drops 4-6 times daily, particularly during environmental stress or screen time, substantially improves comfort.
- Topical anti-inflammatory medications, including mild steroid eye drops, may be prescribed during periods of inflammation. These medications reduce swelling, redness, and associated discomfort, typically providing relief within several days of consistent use. However, prolonged steroid use requires medical supervision to prevent potential complications.
Lifestyle Modifications and Environmental Control
Implementing practical lifestyle changes dramatically reduces symptoms and prevents disease progression.
- Sun Protection: Wearing high-quality sunglasses that block 99-100% of UVA and UVB radiation during outdoor activities provides essential protection. Wide-brimmed hats offer additional protection by reducing direct sunlight exposure to the ocular surface. For those working outdoors, protective eyewear designed for occupational use offers superior coverage compared to standard sunglasses.
- Environmental Modifications: Using humidifiers to maintain indoor humidity between 40-60% prevents excessive dryness, particularly in air-conditioned environments. Avoiding direct air conditioning vents near the face, minimizing exposure to smoke and dust, and protecting eyes during windy conditions further reduces irritation.
- Screen Time Management: Taking regular breaks from digital screens following the 20-20-20 rule—looking at something 20 feet away for 20 seconds every 20 minutes—reduces eye strain and maintains tear film stability. Adequate blinking during computer use prevents tear film disruption.
Advanced Treatments and Surgical Options
- While rare, some cases warrant more advanced intervention. When n pinguecula causes chronic discomfort despite conservative measures or becomes cosmetically concerning, surgical removal may be considered.
- Surgical excision removes the abnormal tissue under local anesthesia using a minimally invasive approach. Conjunctival autografting—transplanting healthy conjunctival tissue to the surgical site—reduces recurrence risk and improves cosmetic outcomes. Studies demonstrate that surgical management with conjunctival autografting not only improves appearance but also significantly enhances associated dry eye symptoms in up to 80% of cases.
- Argon laser photocoagulation represents an alternative treatment for select cases. This procedure uses laser energy to remove the abnormal tissue while minimizing trauma to surrounding structures. Post-operative management includes topical antibiotics and steroids to promote healing and prevent complications.
Prevention: Protecting Your Eyes Long-Term
Given that UV exposure and environmental factors drive pinguecula development, prevention strategies deserve serious consideration.
- Consistent Sun Protection: Begin sun protection habits early in life, not just during sunny seasons. Even winter sun reflects off snow and ice, delivering significant UV radiation. Cloudy days don’t eliminate UV exposure—harmful rays penetrate clouds effectively.
- Occupational Precautions: Those working outdoors should prioritize protective eyewear as essential equipment, similar to other safety gear. Taking breaks in shade, scheduling outdoor work during early morning or late afternoon hours when UV intensity is lower, and remaining hydrated all support eye health.
- Regular Eye Examinations: Annual or biennial comprehensive eye exams allow early detection of pinguecula and other eye conditions. Early identification enables preventive intervention before symptoms develop.
- Nutritional Support: Consuming antioxidant-rich foods, including leafy greens, colorful vegetables, nuts, and omega-3-rich fish, supports overall eye health and may reduce oxidative stress contributing to pinguecula development.
When to Seek Professional Evaluation
Understanding when a professional evaluation becomes necessary ensures the timely management of potential complications. Contact your eye care provider if you notice a new growth on your eye, if existing pinguecula changes in size or color, if discomfort intensifies despite conservative management, or if you develop new visual symptoms. While most changes in pinguecula prove benign, professional evaluation rules out less common conditions requiring specific intervention.
Conclusion: Living Well With Pinguecula
Pinguecula represents a common, generally benign eye condition that rarely threatens vision or overall eye health. Understanding the causes—primarily UV exposure and environmental irritants—empowers individuals to implement effective prevention strategies. While many people live comfortably with asymptomatic pinguecula, those experiencing symptoms benefit from comprehensive management approaches ranging from simple artificial tears to surgical intervention in select cases.