Introduction
Imagine drifting into a peaceful slumber—only to be jolted awake by a sudden gasp for air. For millions worldwide, this nocturnal drama is all too real. Sleep apnea lurks in the shadows of the night, disrupting rest, health, and well-being. But fear not: understanding the causes, recognizing the symptoms, and exploring both traditional and cutting-edge treatments can transform your nights from restless to restorative.
What Is Sleep Apnea?
At its core, sleep apnea is a sleep-related breathing disorder characterized by repeated lapses or pauses in breathing during sleep. Those pauses can last seconds or even minutes, often ending with a choking or snorting sound as normal breathing resumes. There are two primary types:
- Obstructive Sleep Apnea (OSA): When throat muscles relax excessively, the airway narrows or collapses. Loud snoring and daytime fatigue often signal its presence.
- Central Sleep Apnea (CSA): The brain’s communication breakdown with respiratory muscles leads to shallow breathing or pauses—without the telltale snoring.
These disruptions not only shatter sleep quality but also carry serious health consequences if left untreated.
Recognizing the Warning Signs
Sleep apnea’s stealthy nature means many sufferers remain unaware, attributing daytime fatigue or morning headaches to stress. Key symptoms of sleep apnea include:
- Chronic, loud snoring
- Frequent awakenings or gasping episodes
- Morning headaches and dry mouth
- Daytime sleepiness, irritability, or impaired concentration
- Suspected sleep apnea in children may appear as hyperactivity, bedwetting, or behavioral issues.
If you suspect you—or a loved one—may have sleep apnea, a home sleep test offers a convenient starting point. Yet definitive diagnosis relies on a professional sleep study or polysomnography, where sensors monitor breathing, oxygen levels, heart rate, and sleep stages.
Unmasking the Risk Factors
Certain factors raise the curtain on sleep apnea’s performance:
- Age: Risk climbs into your 60s and 70s.
- Sex: Men—particularly in early adulthood—are more prone, though post-menopausal women also see increased incidence.
- Body Weight & Anatomy: A higher BMI, larger tongue, or shorter jaw can contribute to airway obstruction.
- Medical Conditions: Heart failure, stroke, or neurological disorders can precipitate CSA.
- Lifestyle: Chronic opioid use and high-altitude exposure may trigger central sleep apnea.
Understanding these risk factors empowers early detection and proactive care.
From Polysomnography to Personalized Care
Diagnosing sleep apnea typically follows this path:
- Initial Consultation: Discuss symptoms, medical history, and lifestyle.
- At-Home Sleep Test: Portable monitors record breathing events for suspected OSA.
- In-Lab Polysomnography: Gold-standard study in a sleep clinic distinguishes OSA from CSA and gauges severity.
- Professional Interpretation: Sleep specialists analyze data to craft a tailored treatment plan.
Traditional and Advanced Treatments
Treatment goals focus on restoring uninterrupted breathing, improving sleep quality, and mitigating health risks. Options include:
Continuous Positive Airway Pressure (CPAP)
A mask delivers gentle air pressure to keep the airway open—often the first-line therapy for moderate to severe OSA.
Oral Appliances
Custom-fitted mouthpieces reposition the jaw and tongue, easing mild to moderate OSA.
Surgical Interventions
For select cases, procedures such as uvulopalatopharyngoplasty or genioglossus advancement remove or reposition tissue to widen the airway.
Alternative Treatments
Positional therapy encourages side sleeping, while weight management and alcohol reduction can lessen airway collapse.
Emerging therapies—like hypoglossal nerve stimulation—offer hope for those intolerant of CPAP, signaling a new era of innovation.
Navigating Potential Complications
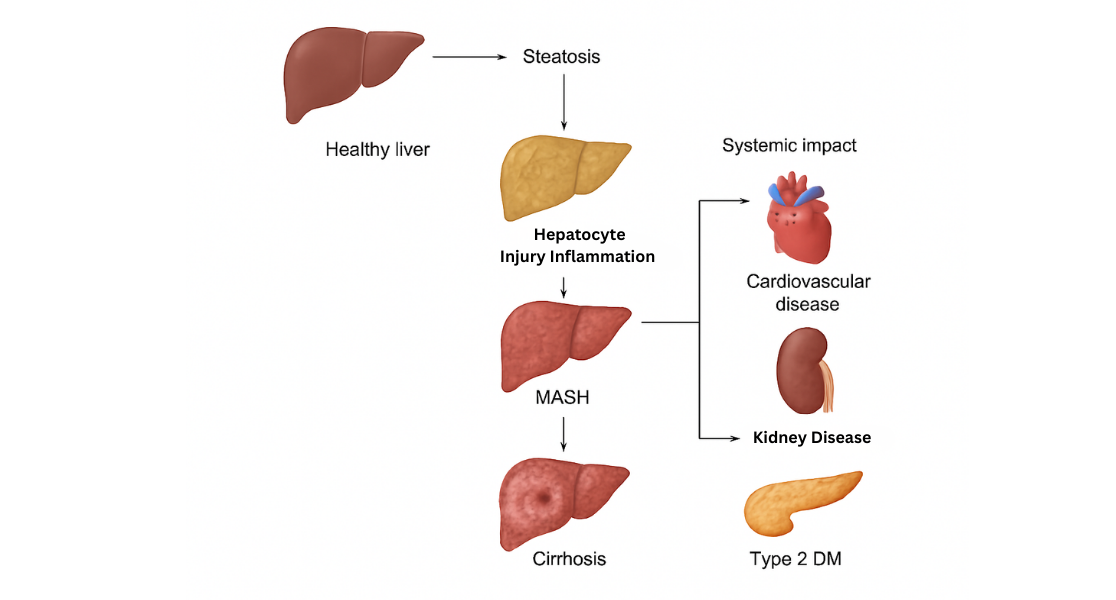
Untreated sleep apnea doesn’t just steal sleep; it invites a host of complications:
- Cardiovascular Disease: Hypertension, stroke, heart failure, and arrhythmias.
- Metabolic Disorders: Elevated risk of type 2 diabetes.
- Pulmonary Hypertension: Strained lung arteries burden the heart.
- Neurocognitive Effects: Memory lapses, concentration problems, and mood disturbances.
- Liver Health: Nonalcoholic fatty liver changes linked to oxygen deprivation.
Prompt treatment is crucial to avert these cascading health risks.
Living Well with Sleep Apnea
Thriving with sleep apnea involves more than devices and surgeries. Embrace these practical strategies:
- Maintain regular follow-up with your sleep specialist to optimize therapy.
- Clean CPAP masks or oral appliances meticulously to prevent irritation or infection.
- Avoid driving or operating machinery when drowsy.
- Experiment with sleep position aids to discourage back sleeping.
- Limit alcohol, especially close to bedtime.
- Inform all healthcare providers of your apnea diagnosis.
Sleep Apnea in Children: A Special Note
While often seen in adults, OSA affects 1–5% of children. Enlarged tonsils, obesity, or craniofacial anomalies may underlie pediatric sleep apnea. Early recognition—through observation of snoring, behavioral changes, or daytime sleepiness—and intervention can safeguard cognitive development and overall health.
Sleep apnea need not stay hidden in the dark. Armed with knowledge of its symptoms, risk factors, and a spectrum of treatment options, you can reclaim restful nights and vibrant days. If you suspect sleep apnea, reach out to a qualified professional—your journey to deeper, healthier sleep begins now.