Introduction
In the quiet landscape of our internal organs, the liver stands as a silent, stoic hero. It’s the body’s master chemist, a tireless filtration plant, and a metabolic powerhouse, performing over 500 vital functions without ever asking for a spotlight. But a silent epidemic is underway, one that is compromising this crucial organ in millions of people who may not even know it. This condition, known as Non-Alcoholic Fatty Liver Disease (NAFLD), is rapidly becoming the most common cause of chronic liver disease worldwide. It’s a stealthy threat, often developing without symptoms, driven not by alcohol, but by the very fabric of our modern lifestyles.
A Hidden Puzzle: The Gut, The Diet, and The Unexpected Truth
The story of NAFLD is complex, a web of genetics, diet, and metabolic health. But what if a crucial part of the story lies hidden in two essential nutrients and the trillions of bacteria residing in our gut? Recent scientific research, exploring a strange and paradoxical diet in mice, has peeled back a new layer of this mystery. The findings are a stark reminder that when it comes to our health, things are rarely as they seem, and the path to understanding disease can take the most unexpected turns. This journey into the liver’s inner workings doesn’t just reveal how a vital organ can fall ill; it illuminates the profound and intricate connections between our diet, our microbiome, and our overall well-being.
1. The Growing Threat: When Your Liver Gets Weighed Down
For decades, liver disease was almost exclusively associated with heavy alcohol consumption or viral hepatitis. But that narrative has fundamentally shifted. Today, the primary threat to liver health for a vast portion of the global population is NAFLD, a condition characterized by the accumulation of excess fat in liver cells. Think of your liver as a high-efficiency processing plant; in NAFLD, this plant becomes clogged with fat, slowing down its operations.
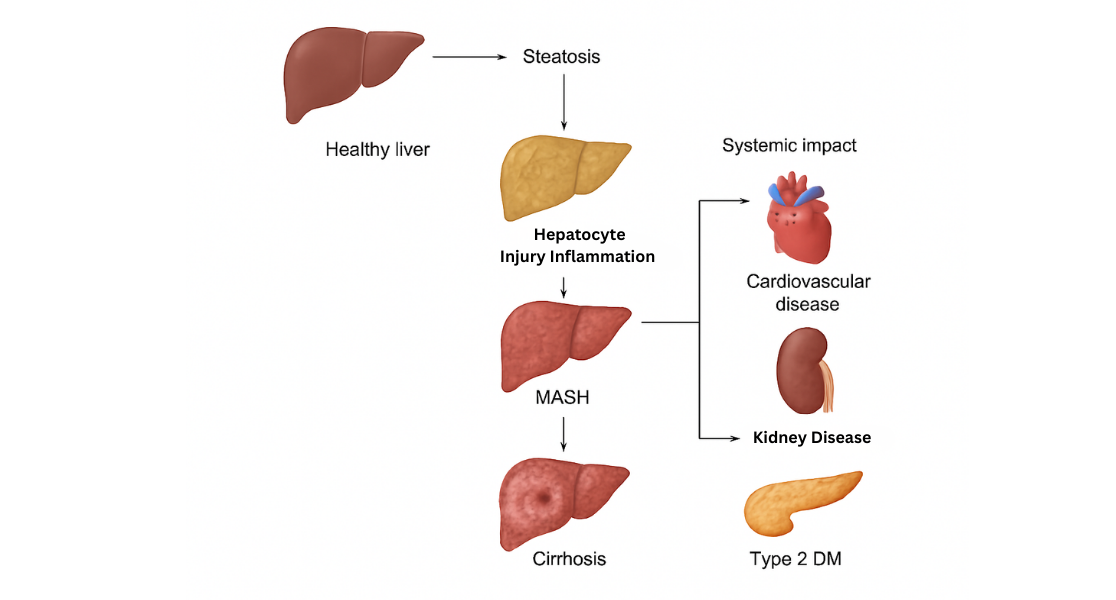
The Deadly Progression: From Inflammation to Scarring
For many, this initial stage, called simple steatosis, is non-progressive. The real danger emerges when NAFLD progresses to Non-Alcoholic Steatohepatitis (NASH). The “-itis” in steatohepatitis means inflammation. In NASH, the excess fat triggers a state of chronic inflammation, which begins to injure and kill liver cells. Over time, this relentless inflammation leads to the formation of scar tissue, a process known as fibrosis. As fibrosis worsens, it can culminate in cirrhosis, a state of severe, often irreversible scarring that dramatically impairs liver function and can lead to liver failure or liver cancer.
The Metabolic Storm: Why Your Liver is Under Attack
What’s driving this alarming trend? This answer intertwines deeply with other modern health crises, particularly metabolic syndrome—a cluster of conditions that includes high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol or triglyceride levels. The presence of insulin resistance, a hallmark of type 2 diabetes and obesity, is a powerful predictor of developing NAFLD. In essence, the liver becomes a casualty of a body struggling to manage its metabolic load, making NAFLD a stark, physical manifestation of a systemic problem.
2. The Unsung Heroes: Two Nutrients Your Liver Craves
In the intricate biochemistry of our bodies, certain compounds are so vital that they are deemed “essential.” Our bodies cannot produce them in sufficient quantities, so we must obtain them from our diet. Two such unsung heroes, particularly for liver health, are methionine and choline.
Methionine: The Master of Detoxification
Methionine is an essential amino acid, a building block for proteins. But its role extends far beyond that. It is a critical component in a process called methylation, which is vital for everything from DNA repair to detoxification pathways in the liver. It helps produce the body’s primary antioxidant, glutathione, which protects cells from damage. You can find methionine in protein-rich foods like meat, fish, and dairy products, as well as in nuts and seeds.
Choline: The Essential Fat-Traffic Controller
Choline, while not technically a vitamin, is an essential vitamin-like nutrient that plays a central role in fat metabolism. One of its most critical jobs is to help produce phosphatidylcholine, a type of fat that is necessary to package and transport triglycerides (a type of fat) out of the liver. Without enough choline, fat gets “trapped” in the liver, leading directly to the fatty liver condition known as steatosis. Choline is also the precursor to the neurotransmitter acetylcholine, which is crucial for memory, mood, and muscle control. Rich dietary sources of choline include egg yolks, beef liver, soybeans, chicken, fish, and shiitake mushrooms.
The Dangerous Link: How Deficiency Sparks Disease
Decades of research have established a clear link: diets deficient in these two nutrients reliably induce fatty liver and liver damage in both animals and humans. This foundational knowledge set the stage for a fascinating recent experiment designed to explore the deeper mechanisms of liver disease.
3. The Skinny Fat Paradox: A Bizarre Diet Reveals a Gut-Liver Twist
Scientists often use highly specific, controlled diets in animal models to understand the precise mechanisms of disease. A recent study published in Biochimica et Biophysica Acta – Molecular and Cell Biology of Lipids utilized one such model: a diet completely deficient in methionine and choline (an MCD diet), which was fed to a group of mice for 10 weeks. The goal was to map the comprehensive changes that led from a simple nutrient deficiency to full-blown NASH.
The Hidden Devastation: Inside the Liver’s Collapse
As expected, the MCD diet wreaked havoc on the mice’s livers. The organ showed classic signs of severe NASH, including massive fat accumulation (steatosis), widespread inflammation, and the activation of genes associated with fibrosis (scarring). The damage was undeniable and severe, mirroring the worst stages of liver disease. However, while the liver was failing, the diet produced a series of deeply paradoxical effects on the rest of the body that baffled researchers.
The “Skinny Fat” Paradox: A deceptive Exterior
The mice on the MCD diet actually lost significant body weight and fat mass. Furthermore, their blood tests showed a surprising improvement in several metabolic markers: their plasma levels of triglycerides, cholesterol, glucose, and insulin all decreased. This created a “skinny fat” paradox. On the outside and according to their blood work, the mice appeared metabolically healthier. They were leaner and had lower cholesterol and blood sugar. Yet, inside their bodies, their livers were screaming in distress, suffering from the exact type of severe disease often associated with obesity and metabolic syndrome in humans. This disconnect was the first major clue that the MCD diet was triggering a unique pathway of disease.
Decoding the Microbiome: A Shift in the Bacterial Balance
The researchers dug deeper, employing advanced “OMICS” techniques to analyze the mice’s complete lipid, metabolite, and gut microbiome profiles. The results from the gut were particularly striking. The microbiome of the MCD-fed mice had been dramatically altered. There was a significant increase in the phylum Firmicutes and a sharp decrease in Bacteroidetes and Actinobacteria. This shift is a classic sign of gut dysbiosis, a severe imbalance in the gut’s microbial community that disrupts the body’s internal ecosystem.
The Leaky Gut Connection: How Dysbiosis Poisons the Liver
The gut and the liver are intricately connected through the gut-liver axis, a bidirectional highway primarily linked by the portal vein, which carries blood directly from the digestive system to the liver. A healthy gut lining acts as a tight barrier, but in a state of dysbiosis, this barrier can become more permeable—a condition often called “leaky gut.” When this happens, bacterial components and inflammatory molecules can “leak” from the gut and travel directly to the liver, triggering an immune response and promoting inflammation. The study’s findings strongly suggested this gut-liver connection was a key player in the development of NASH in these mice.
The Final Twist: A Different Path to the Same Disease
After meticulously mapping the profound changes in lipids, amino acids, and bile acids, the scientists came to a startling conclusion. Although the MCD diet successfully induced a state of NASH that visually resembled the human disease, the underlying molecular and metabolic mechanisms were fundamentally different. In humans, NASH is typically driven by an overload of calories, leading to obesity and insulin resistance, which then overwhelms the liver with fat. In this mouse model, the disease was driven by a specific nutrient deficiency that, despite causing weight loss, initiated a toxic cascade involving gut dysbiosis and altered metabolic pathways that ultimately converged on the same endpoint: a fatty, inflamed, and scarred liver.
4. Why This Mouse Study Matters for You
It’s easy to dismiss a mouse study, especially one that concludes the mechanism isn’t the same as in humans. But doing so would miss the profound implications of this research. This study is critically important not because it offers a direct model of human NASH, but because it brilliantly illuminates the complexity of liver health and provides three crucial insights.
- It Confirms Nutrients are Non-Negotiable: The research powerfully reinforces the fact that essential nutrients like methionine and choline are absolutely fundamental to liver function. It demonstrates that a severe deficiency can be just as damaging as a caloric excess, albeit through a different biological route. It’s a stark reminder that “health” isn’t just about avoiding a “bad” diet; it’s also about ensuring you get enough of the “good” stuff.
- It Puts the Gut-Liver Axis in the Spotlight: The study adds to a growing mountain of evidence that gut health is inextricably linked to liver health. The finding that a simple dietary change could so dramatically alter the gut microbiome—which in turn contributed to severe liver disease—underscores the importance of maintaining a balanced gut ecosystem. Your liver is directly downstream from your gut, meaning it’s one of the first organs to face the consequences of gut-based inflammation.
- It Shows That “Healthy” Metrics Can Be Deceiving: The most striking takeaway is the paradox itself. The mice were losing weight and had “better” numbers for cholesterol and glucose, all while developing a life-threatening disease. This is a crucial lesson in our modern, data-obsessed approach to health. Body weight, BMI, and even standard blood panels do not always tell the whole story. True health is about cellular function and metabolic balance, not just numbers on a scale or a lab report.
5. Actionable Steps to Protect Your Body’s Hero
While you are not a mouse on an extreme experimental diet, the principles uncovered in this research offer a clear roadmap for supporting your liver. The goal is to avoid both caloric overload and nutrient deficiency, creating a stable internal environment where your liver can thrive.
- Prioritize Nutrient-Rich Foods: Ensure your diet includes ample sources of methionine and choline. Eggs, lean meats, fish, soy products, and cruciferous vegetables like broccoli and Brussels sprouts are excellent choices.
- Nourish Your Gut: Support a healthy gut microbiome by eating a diet rich in fiber from a diverse range of plants. Fermented foods like yogurt, kefir, and kimchi can also introduce beneficial bacteria.
- Maintain a Healthy Weight: Excess weight and obesity are the primary drivers of NAFLD in humans, so achieving and maintaining a healthy weight through a balanced diet and regular exercise is the single most effective strategy for protecting your liver.
- Limit Processed Foods and Sugars: Diets high in processed carbohydrates, sugary drinks, and unhealthy fats are known to promote fat accumulation in the liver. Focus on whole, unprocessed foods.
Conclusion: A New Chapter in Liver Health
The journey into the world of a methionine- and choline-deficient mouse diet does not end with a simple answer. Instead, it leaves us with a deeper appreciation for the elegant complexity of our own bodies. This study reveals that a single factor does not govern our liver’s health. Instead, a delicate interplay between what we eat, our gut health, and our overall metabolic state determines it. Although the liver may cry for help silently, we can learn to listen more closely by understanding these connections. We can then take proactive steps to protect this vital organ long before pain or disease forces it to scream.